When patients struggle or aren’t able to self-report their pain, it can make it difficult to assess pain levels. Below are some validated observational tools for assessing pain in non-verbal clients, clients with cognitive impairments, and children.
| Rating System | The Faces Pain Scale uses drawn faces to represent pain levels on a scale of 0 to 5. |
|---|---|
| Common Use | Most commonly used with children aged 3+, may also be used for adults with cognitive impairments. |
| Instructions | This scale is intended to measure how the patient feel inside, not how their face looks. The pain scale is shown to the patient with these instructions: “These faces show how much something can hurt. This face [point to face above number “0”] shows no pain. The faces show more and more pain up to this one [point to the face above number “5”] – it shows very much pain. Point to the face that shows how much you hurt [right now].” |
| 0 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
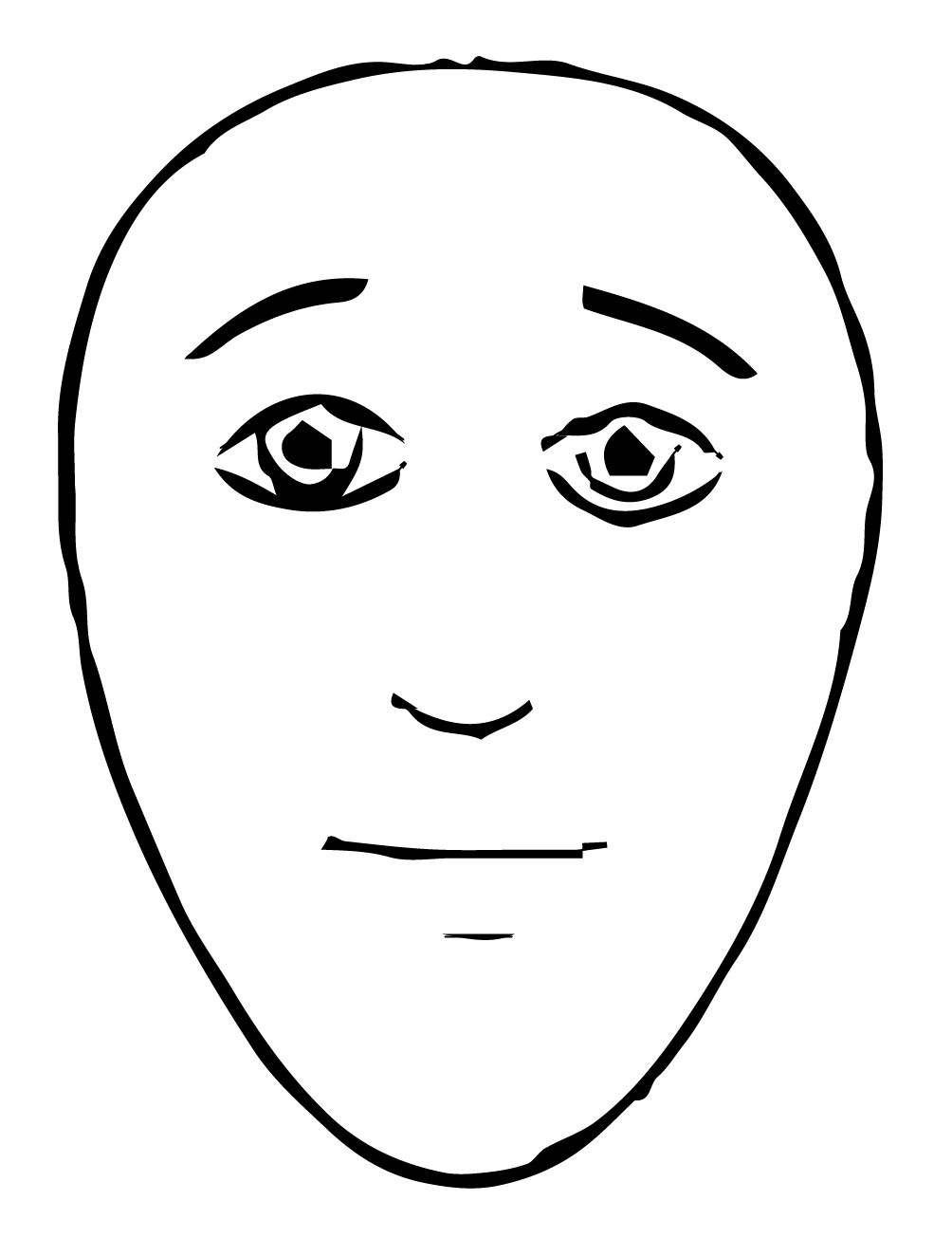 |
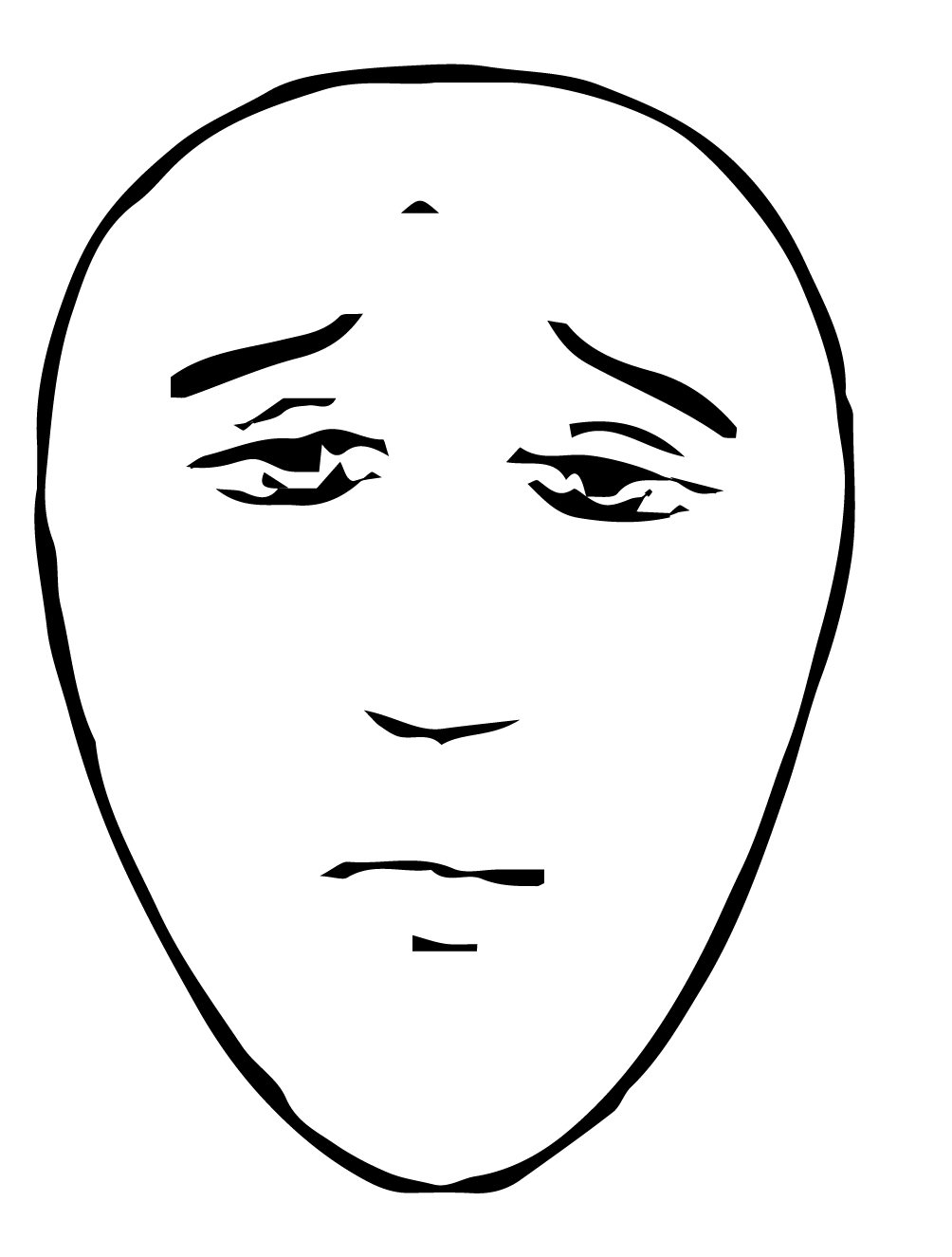 |
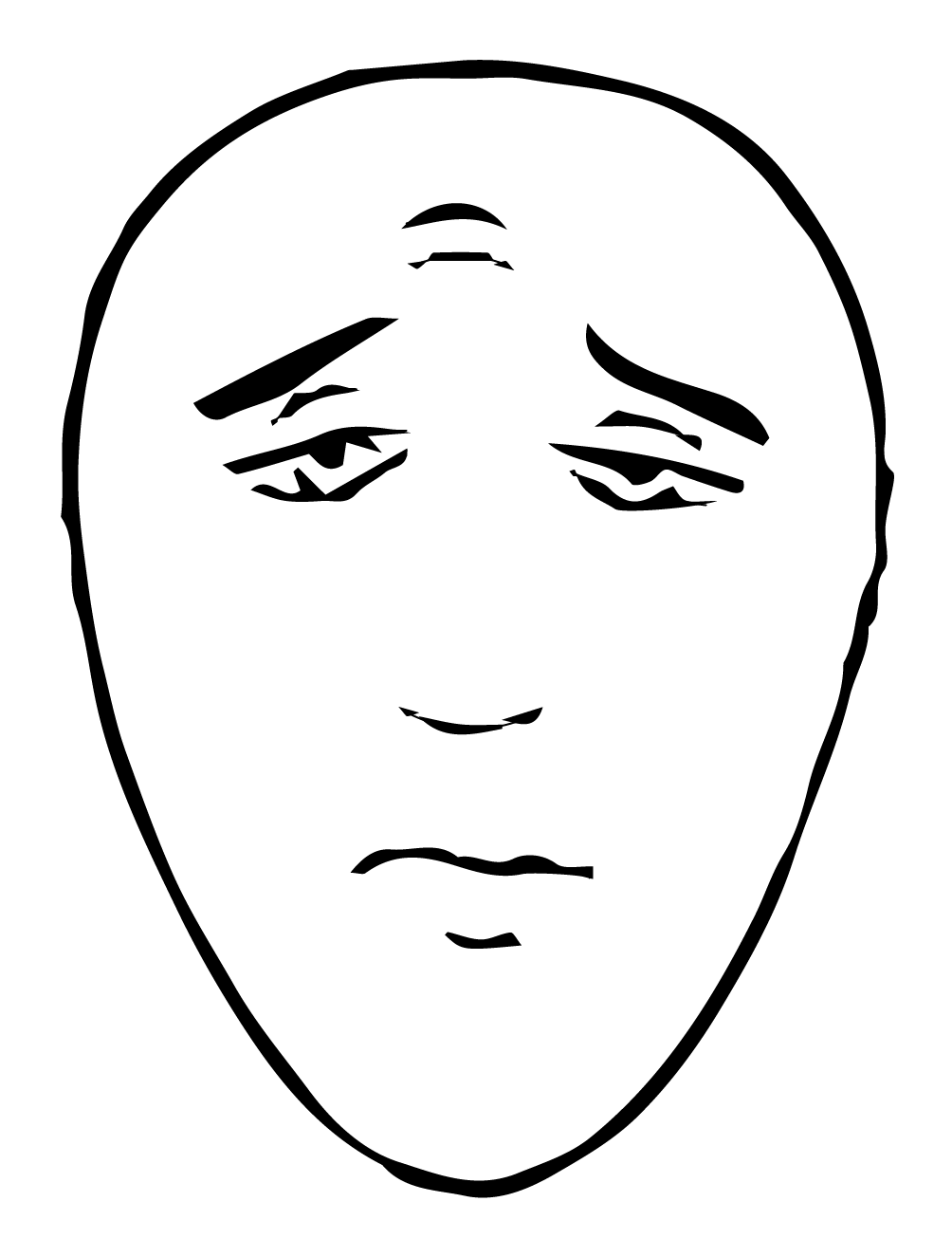 |
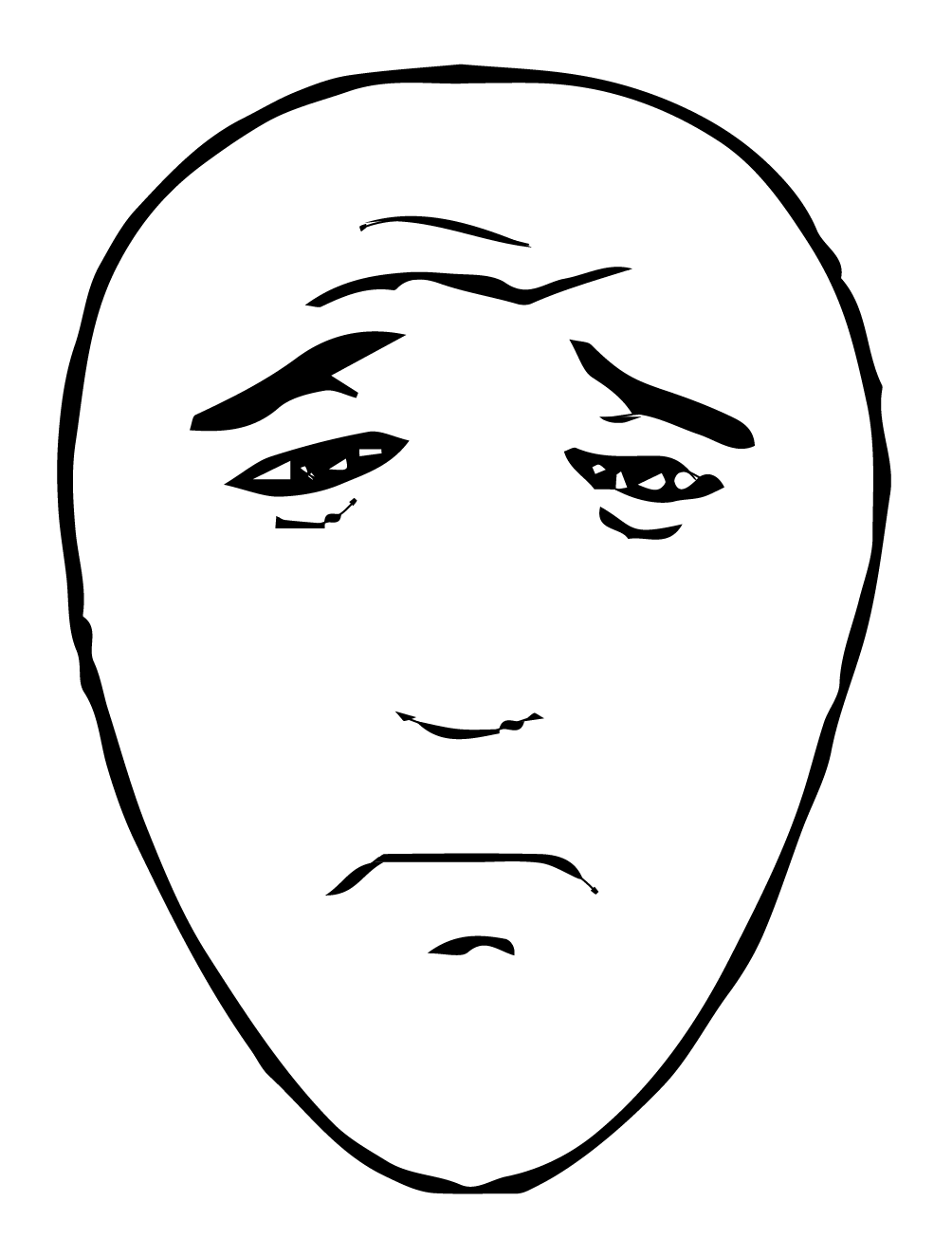 |
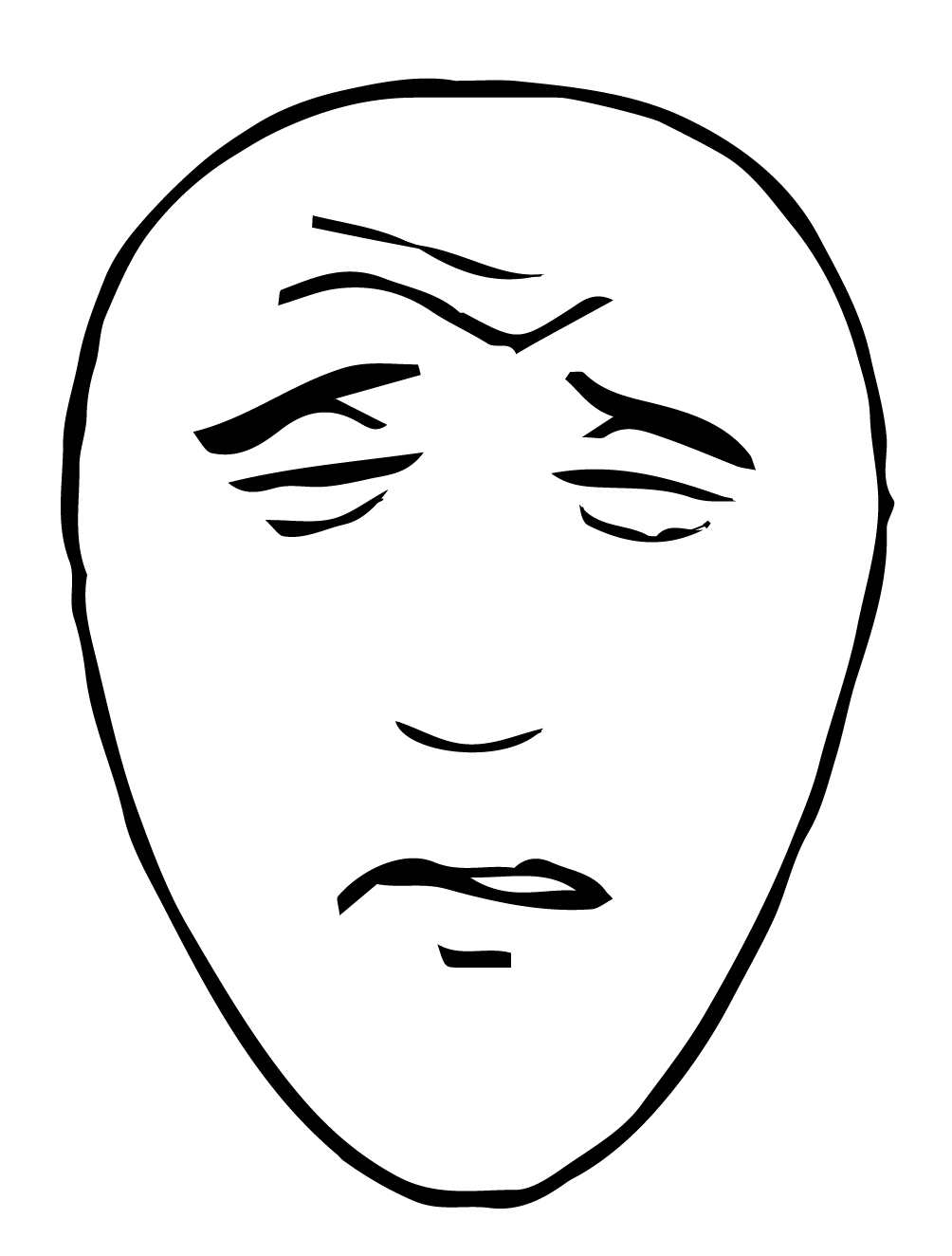 |
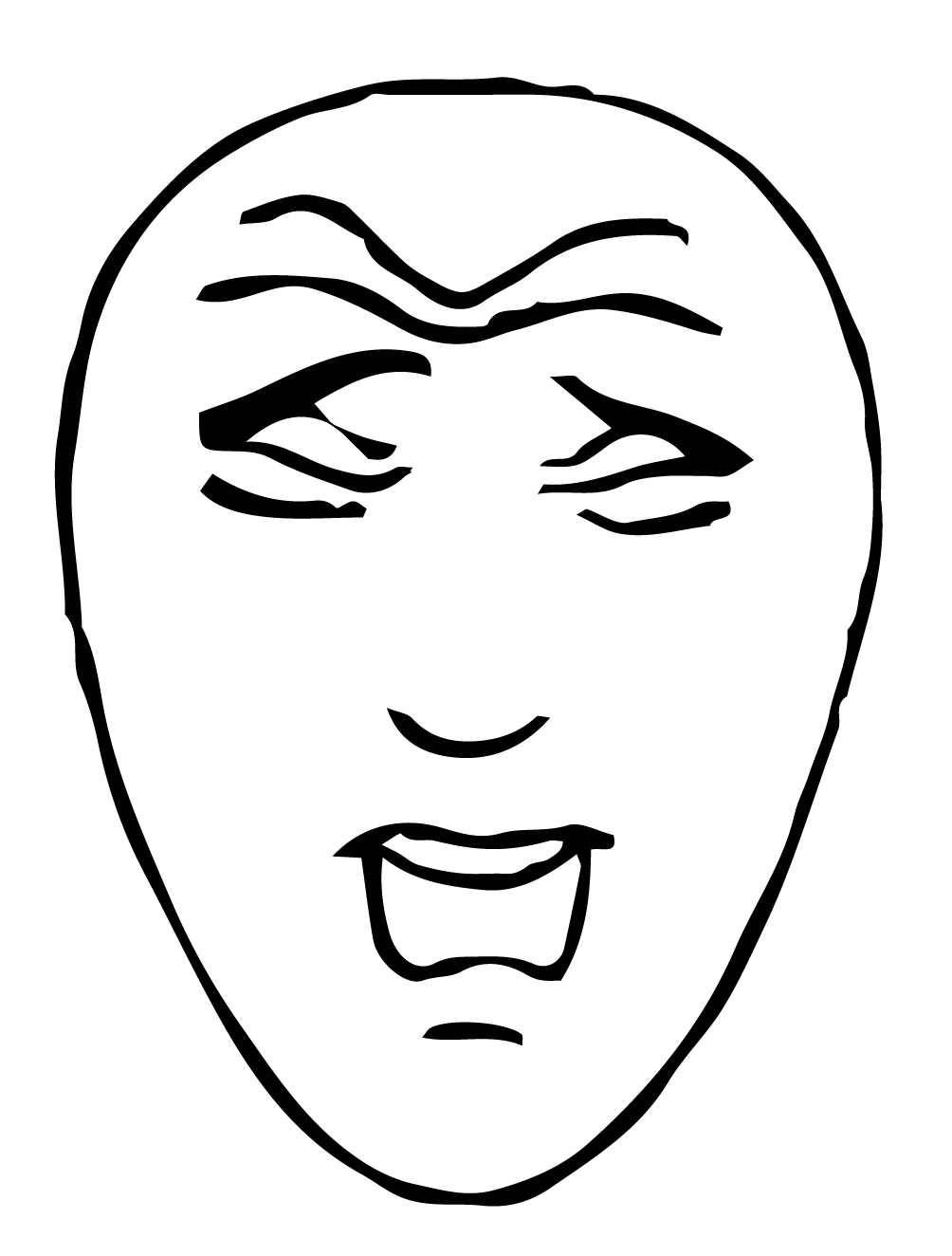 |
Source: Hicks, C. L., von Baeyer, C. L., Spafford, P. A., van Korlaar, I., & Goodenough, B. (2001). The Faces Pain Scale – Revised: Toward a common metric in pediatric pain measurement. Pain, 93, 173-83.
| Rating System |
|---|
| The Faces Pain Scale uses drawn faces to represent pain levels on a scale of 0 to 5. |
| Common Use |
| Most commonly used with children aged 3+, may also be used for adults with cognitive impairments |
| Instructions |
| This scale is intended to measure how the patient feel inside, not how their face looks. The pain scale is shown to the patient with these instructions: “These faces show how much something can hurt. This face [point to face above number “0”] shows no pain. The faces show more and more pain up to this one [point to the face above number “5”] – it shows very much pain. Point to the face that shows how much you hurt [right now].” |
| Number | Visual |
|---|---|
| 0 | 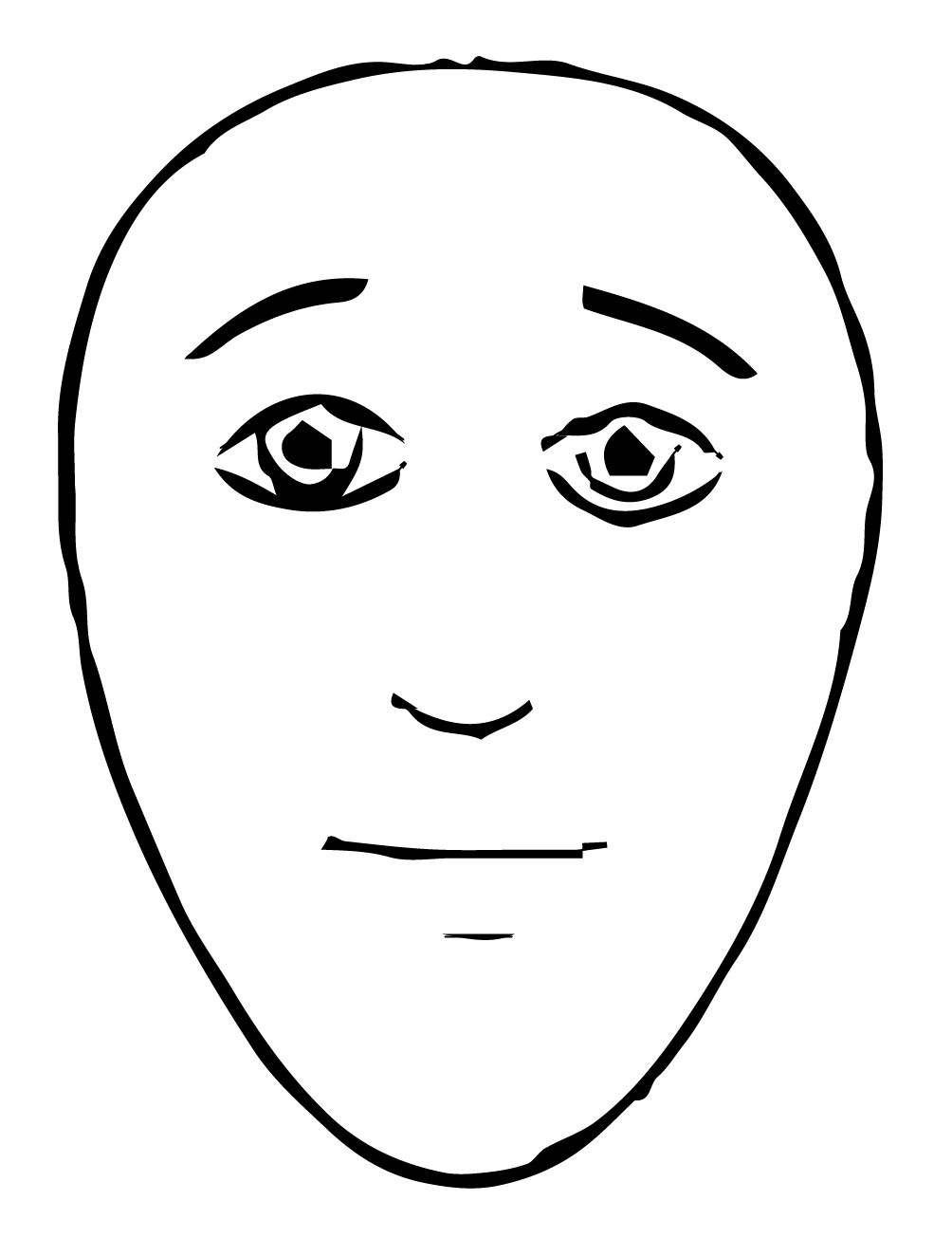 |
| 1 | 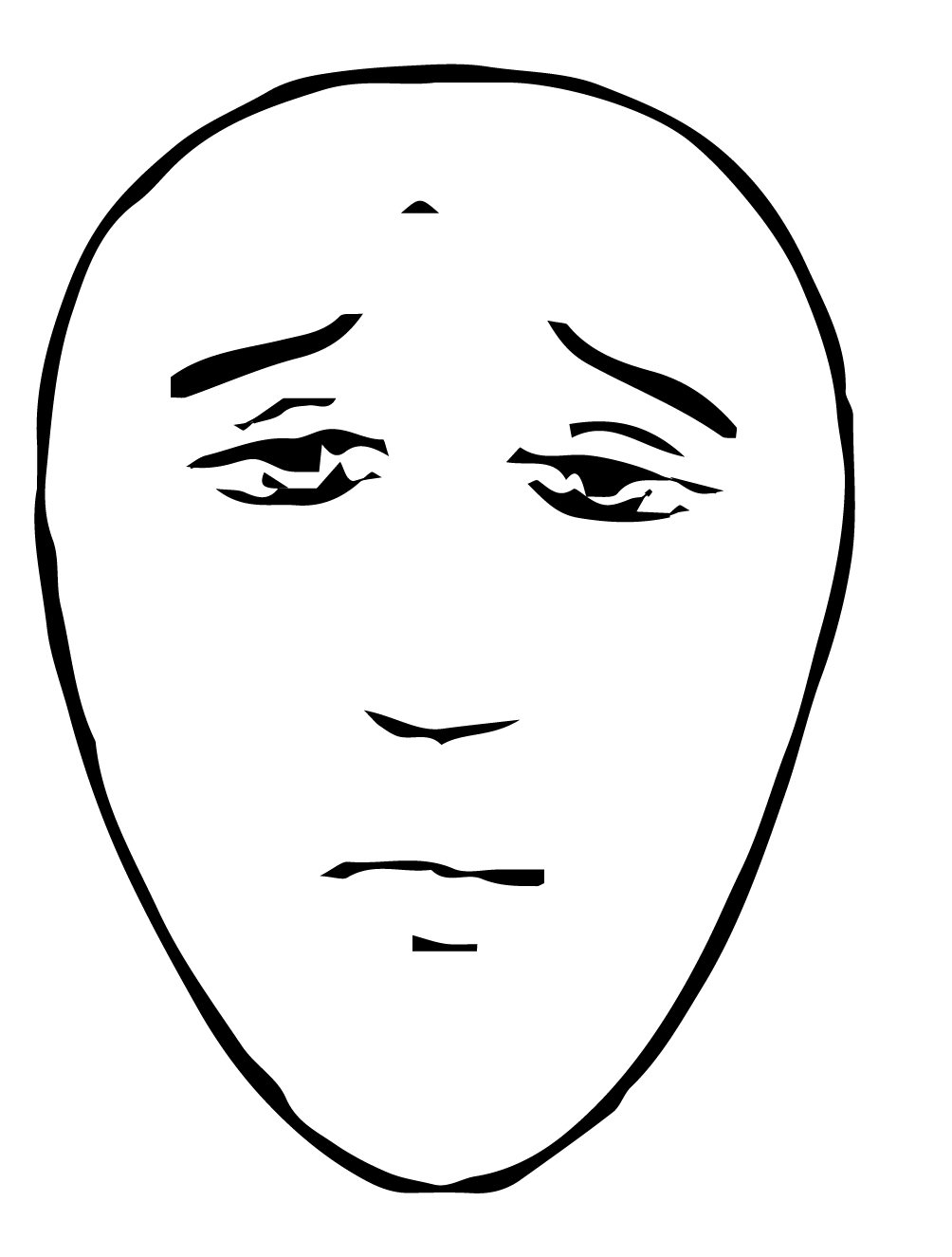 |
| 2 | 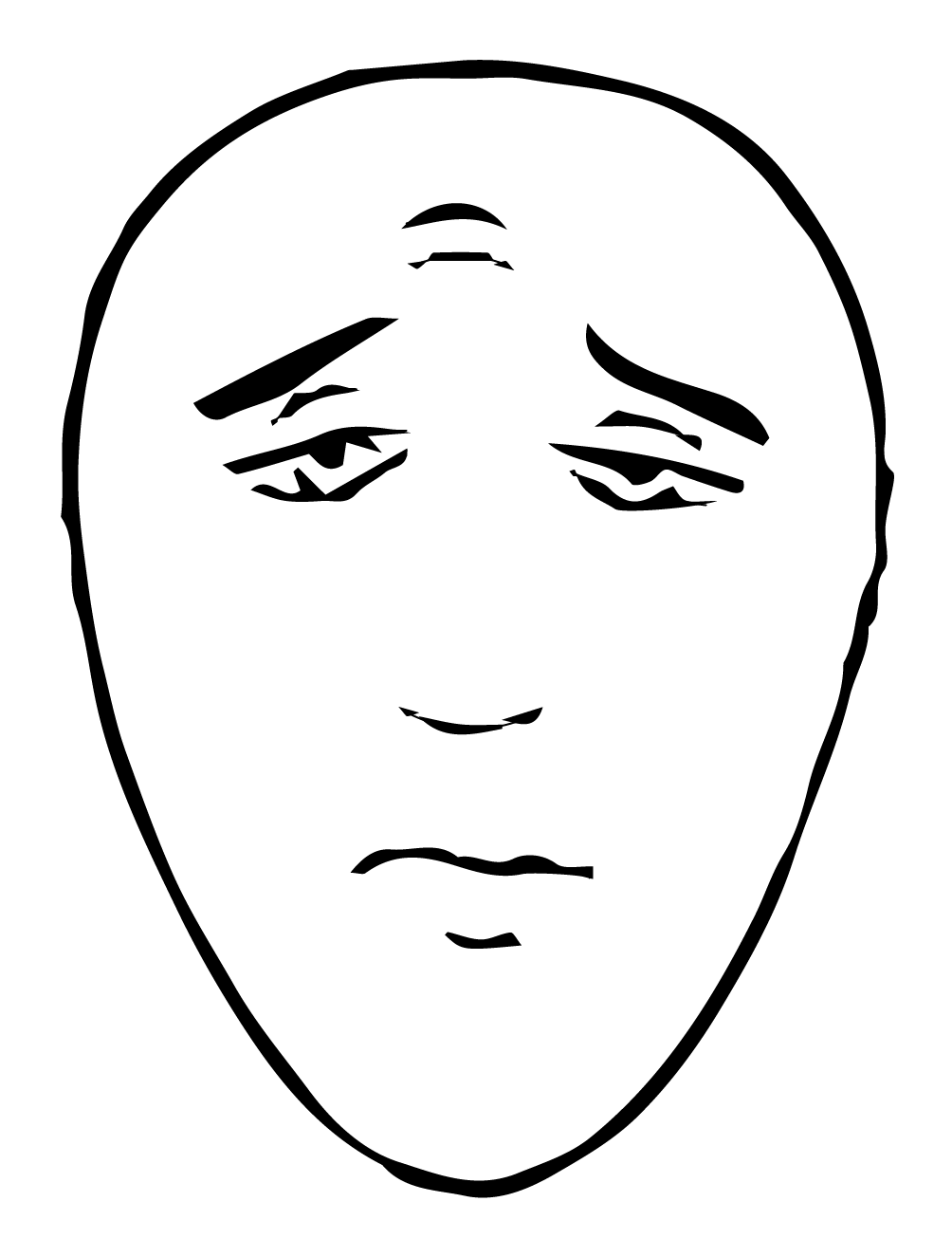 |
| 3 | 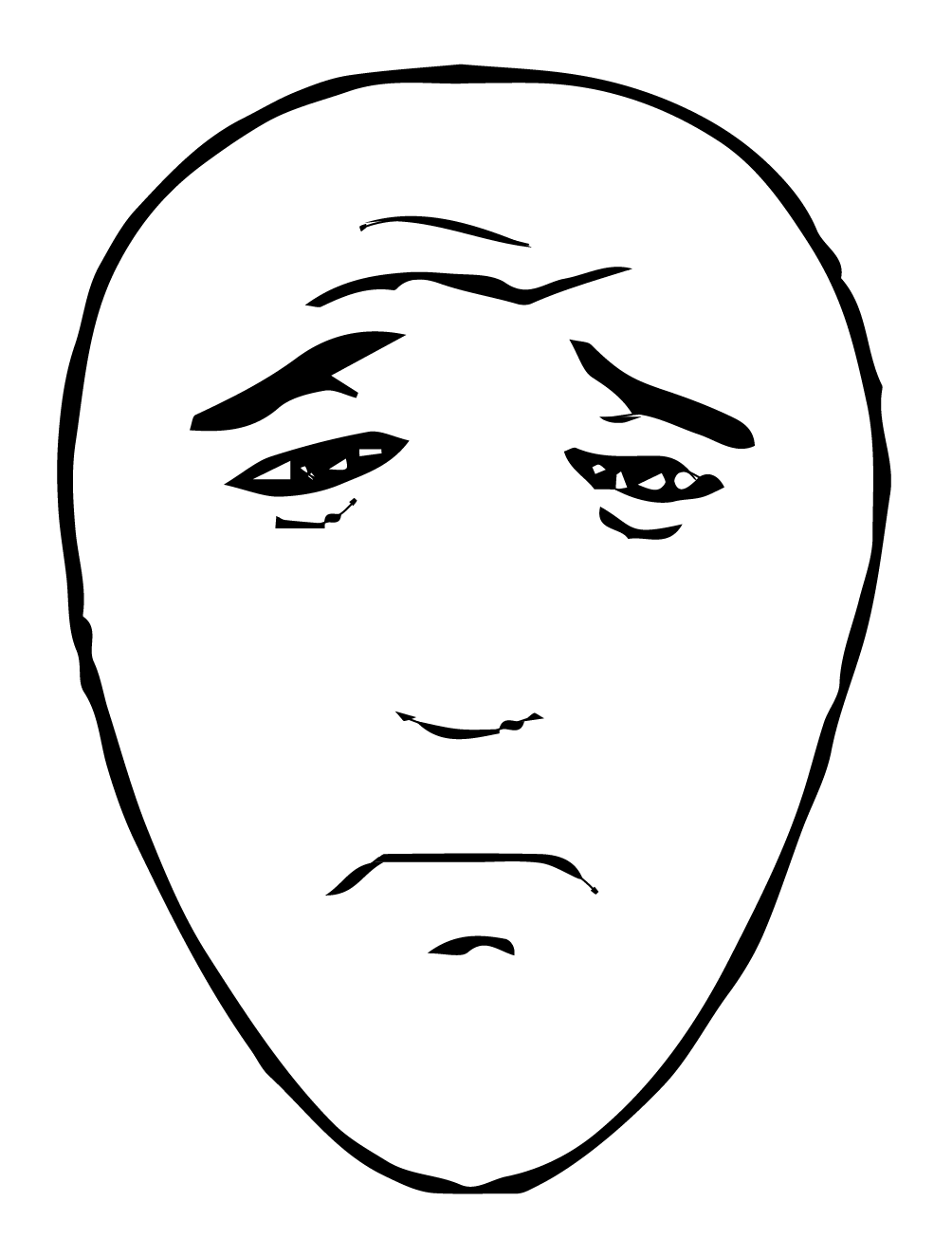 |
| 4 | 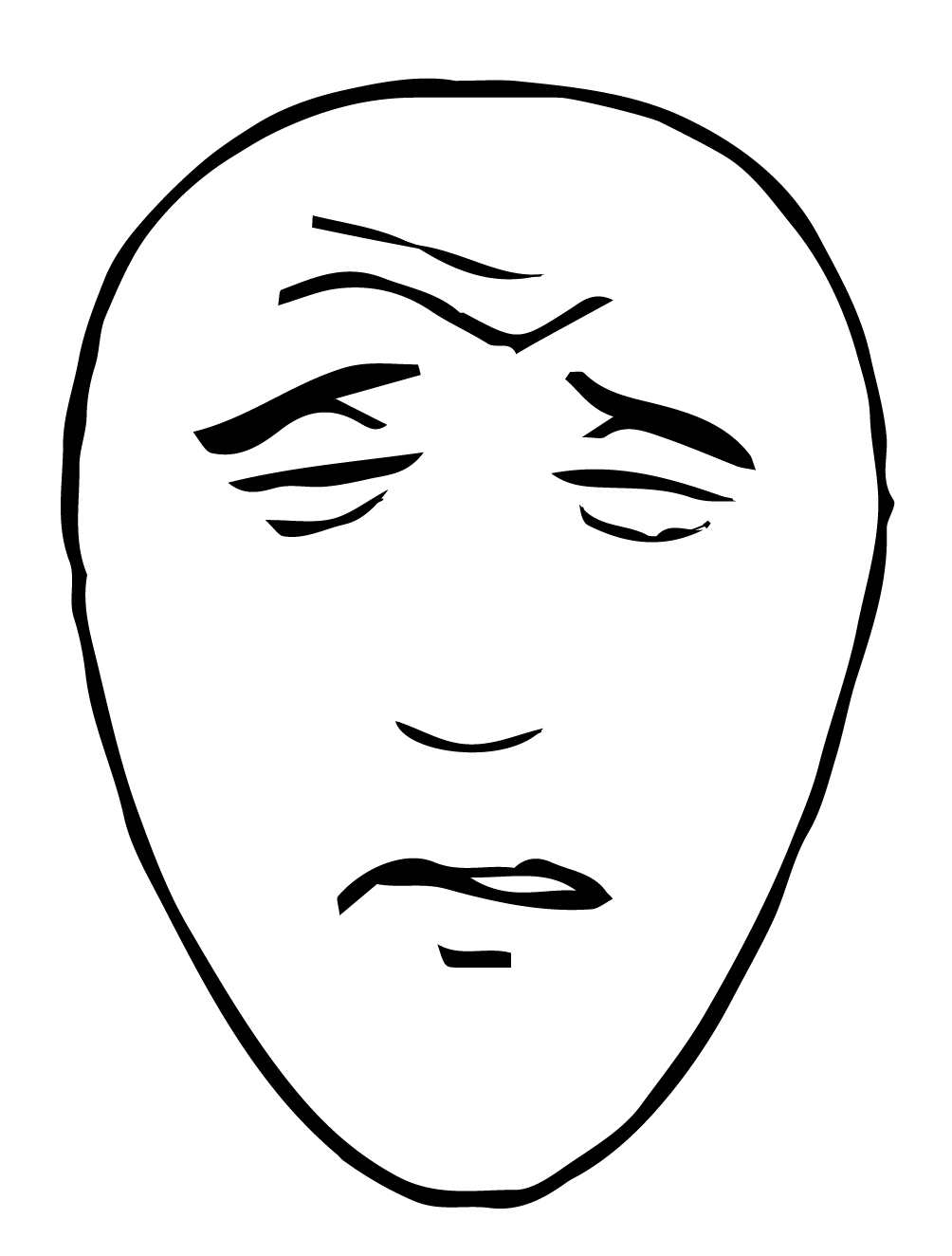 |
| 5 | 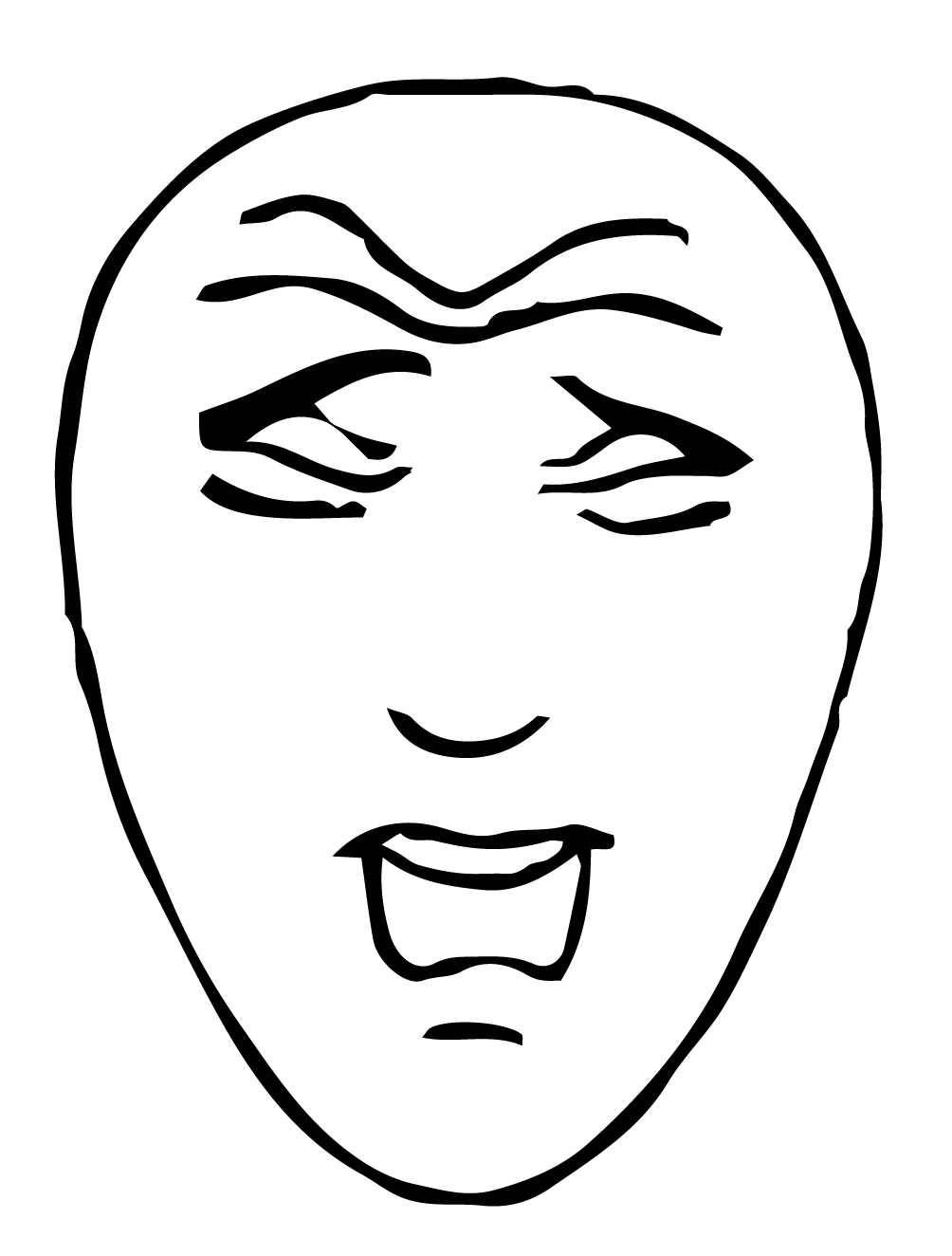 |
Source: Hicks, C. L., von Baeyer, C. L., Spafford, P. A., van Korlaar, I., & Goodenough, B. (2001). The Faces Pain Scale – Revised: Toward a common metric in pediatric pain measurement. Pain, 93, 173-83.
| Rating System | FLACC stands for face, legs, activity, crying, and consolability. A total score is calculated by rating each category on a scale between 0 to 2. The result is a total score out of 10: Scale of 0 to 10, 0=no pain, 10=worst pain possible |
|---|---|
| Common Use | Children under the age of three, non-verbal adults, adults with cognitive impairments. |
| Instructions | Rate the patient in each of the 5 categories and add up the score. |
| 0 | 1 | 2 | |
|---|---|---|---|
| Face | No particular expression or smile. | Occasional grimace or frown, withdrawn, disinterested, sad, appears worried. | Frequent to constant quivering chin, clenched jaw, distressed looking face, expression of fright/panic. |
| Legs | Normal position or relaxed; usual tone and motion to limbs. | Uneasy, restless, tense, occasional tremors. | Kicking, or legs drawn up, marked increase in spasticity, constant tremors, jerking. |
| Activity | Lying quietly, normal position, moves easily, regular, rhythmic respirations. | Squirming, shifting back and forth, tense, tense/guarded movements, mildly agitated, shallow/ splinting respirations, intermittent sighs. | Arched, rigid or jerking, severe agitation, head banging, shivering, breath holding, gasping, severe splinting. |
| Cry | No cry (awake or asleep). | Moans or whimpers:occasional complaint, occasional verbal outbursts, constant grunting. | Crying steadily, screams or sobs, frequent complaints, repeated outbursts, constant grunting. |
| Consolability | Content, relaxed. | Reassured by occasional touching,hugging, or being talked to; distractible. | Difficult to console or comfort, pushing caregiver away, resisting care or comfort measures. |
Malviya, S., Vopel-Lewis, T. Burke, Merkel, S., Tait, A.R. (2006). The revised FLACC Observational Pain Tool: Improved Reliability and Validity for Pain Assessment in Children with Cognitive Impairment. (Pediatric Anesthesia 16: 258-265).
| Rating System |
|---|
| FLACC stands for face, legs, activity, crying, and consolability. A total score is calculated by rating each category on a scale between 0 to 2. The result is a total score out of 10: Scale of 0 to 10, 0=no pain, 10=worst pain possible |
| Common Use |
| Children under the age of three, non-verbal adults, adults with cognitive impairments. |
| Instructions |
| Rate the patient in each of the 5 categories and add up the score. |
| 0 | No particular expression or smile. |
|---|---|
| 1 | Occasional grimace or frown, withdrawn, disinterested, sad, appears worried. |
| 2 | Frequent to constant quivering chin, clenched jaw, distressed looking face, expression of fright/panic. |
| 0 | Normal position or relaxed; usual tone and motion to limbs. |
|---|---|
| 1 | Uneasy, restless, tense, occasional tremors. |
| 2 | Kicking, or legs drawn up, marked increase in spasticity, constant tremors, jerking. |
| 0 | Lying quietly, normal position, moves easily, regular, rhythmic respirations. |
|---|---|
| 1 | Squirming, shifting back and forth, tense, tense/guarded movements, mildly agitated, shallow/ splinting respirations, intermittent sighs. |
| 2 | Arched, rigid or jerking, severe agitation, head banging, shivering, breath holding, gasping, severe splinting. |
| 0 | No cry (awake or asleep). |
|---|---|
| 1 | Moans or whimpers:occasional complaint, occasional verbal outbursts, constant grunting. |
| 2 | Crying steadily, screams or sobs, frequent complaints, repeated outbursts, constant grunting. |
| 0 | Content, relaxed. |
|---|---|
| 1 | Reassured by occasional touching,hugging, or being talked to; distractible. |
| 2 | Difficult to console or comfort, pushing caregiver away, resisting care or comfort measures. |
Malviya, S., Vopel-Lewis, T. Burke, Merkel, S., Tait, A.R. (2006). The revised FLACC Observational Pain Tool: Improved Reliability and Validity for Pain Assessment in Children with Cognitive Impairment. (Pediatric Anesthesia 16: 258-265).
Depending on the severity of the pain, you may want to consider using non-narcotic as well as narcotic options of pain relief. Non-medicinal treatment options — like RICE: rest, ice, compression, elevation — can provide relief of injured areas or limbs. Distraction techniques, such as meditation and deep breathing exercises, may also help alleviate pain.
Changes in vital signs — such as an increased heart rate or blood pressure — can indicate increased pain. It can also indicate decreased oxygen saturation that’s associated with narcotized patients.
It’s important to understand the difference between acute and chronic pain:
| Acute Pain | A sudden onset of pain typically as a result of tissue damage, usually temporary in nature such as surgery, bone fracture, burns, lacerations, etc. |
|---|---|
| Chronic Pain | Lasts longer than 6 months, where pain signals remain active in the nervous system for months or years such as headaches, back pain, fibromyalgia, etc. |
Some topics of conversation are difficult to initiate in virtual settings. Ask your client’s permission to discuss difficult topics or when transitioning to new topics.
Providing emotional support to clients can be more challenging in virtual environments. Virtual care may make it harder to read clients’ emotions and demonstrate empathy for them. We’re also not able to use non-verbal supports like touch. To overcome these challenges:
This website was developed by a team of researchers at the Daphne Cockwell School of Nursing at Toronto Metropolitan University (Formerly Ryerson University). The purpose of the site is to provide supplementary resources for implementing RNAO’s Best Practice Guidelines. Some information about the best practice guidelines has been collected directly from the RNAO BPG website. We have done our best to ensure accuracy, however some discrepancies may occur. For official, up-to-date information about the best practice guidelines, please refer to the RNAO website.